Effects of Bach Flower Remedies on Menopausal Symptoms and Sleep Pattern: A Case Report
Marcele Siegler, PT, BSc; Cristina Frange, PT, MSc; Monica Levy Andersen, BMSc, PhD;
Sergio Tufik, MD, PhD; Helena Hachul, MD, PhD
ABSTRACT
Context • During the postmenopausal stage, women go through many remarkable changes, including physical, emotional, and hormonal. They also experience some unwanted effects, such as vasomotor symptoms, anxiety, and insomnia. The use of Bach flower remedies has been described as a supporting therapy for those symptoms.
Objectives • The investigation aimed to evaluate the effects of the supplement on sleep pattern (ie, sleep perception and objective sleep) and on menopausal symptoms.
Design • The research team created a case report.
Setting • The study was conducted at the Menopause Transition and Postmenopause Sleep Disorder Clinic at the Department of Gynecology of the Federal University of São Paulo in São Paulo, Brazil.
Participant • The participant was a 53-y-old, single woman, at the postmenopausal stage, who had been diagnosed with insomnia according to the criteria of the American Academy of Sleep Medicine and complained of climacteric symptoms.
Intervention • The patient underwent treatment with a blend of the supplement for 4 mo.
Outcome Measures • Sleep questionnaires were given and polysomnography was performed before and after treatment.
Results • Both sleep perception and objective sleep were improved. The patient's anxiety and menopausal symptoms were reduced after the treatment with the supplement.
Conclusion • The use of Bach flower remedies as a therapeutic strategy to relieve menopausal symptoms, such as anxiety, mood changes, and insomnia, seems worthy of further investigation. (Altern Ther Health Med. 2017;23(2):44-48.)
Marcele Siegler, PT, BSc, is an MSc student; Cristina Frange, PT, MSc, is a PhD student; Monica Levy Andersen, BMSc, PhD, is an associate professor and researcher; and Sergio Tufik, MD, PhD, is a professor and researcher in the Department of Psychobiology, Universidade Federal de São Paulo (UNIFESP). in São Paulo, Brazil. Helena Hachul, MD, PhD, is head of sleep disorders in women in the Department of Psychobiology and Department of Gynecology, UNIFESP.
Corresponding author: Helena Hachul, MD, PhD
E-mail address: helenahachul@gmail.com
During the postmenopausal stage, women go through many remarkable changes, including physical, emotional, and hormonal ones. They also experience some unwanted effects, such as vasomotor symptoms (eg, hot flushes and night sweats; substantial mood changes—anxiety and depression; musculoskeletal pain; vaginal dryness; and poor sleep). In addition, the symptoms can lead to alterations in sleep patterns.1 Another symptom in the population is insomnia, characterized as a sleep disorder related to reduced quality and/or quantity of satisfactory sleep, which affects the performance of daily activities.2
Many treatments have been proposed for insomnia, including sleep restrictions and various types of pharmacological treatments, such as hormone therapy. Due to the possible side effects of conventional drugs, the search for nonpharmacological therapies has been increasing.
The number of studies in the area is growing as are the therapeutic options available for the postmenopausal period of women's lives. Some studies have shown that nonpharmacological therapies can produce significant results in decreasing the symptoms of menopause.3-5 Evidence exists for the use of Bach flower remedies as a complementary therapy for menopausal symptoms.6-8
Therapies based on the use of extreme dilutions of flower material began with the seminal studies of Dr Edward Bach, who developed treatments composed of a group of 38 flower tinctures.9 Bach advocated that illness stemmed initially from the emotional field and migrated to the physical field in the form of somatic disease. His therapy can treat various types of functional and organic disorders.6 The compounds are safe and nontoxic and can be used by everyone from little children to older adults. Moreover, the therapy is easy to use and low in cost, with good acceptance by patients.6,9
In that context, the use of Bach flower remedies is a possibility as a nonpharmacological treatment and has been described in the literature as a complementary therapy for menopausal symptoms.6-8 Although not enough conclusive evidence is available yet about the efficacy of Bach flower remedies, the outcomes to date have been promising, making the evaluation of the supplement's benefits an interesting field of research and offering possible improvements in health and quality of life of women. Thus, the current case study evaluates ability of Bach flower remedies to improve the quality of sleep, menopausal symptoms, and, consequently, quality of life in a postmenopausal woman with insomnia.
METHODS
Participant
The participant was a 53-year-old, single woman who sought treatment for insomnia at the Menopause Transition and Postmenopause Sleep Disorder Clinic at the Department of Gynecology of the Federal University of São Paulo (UNIFESP), in São Paulo, Brazil. She was invited by the research team to participate in the study. She was not using any sleep medications, depressive medications, or hormone replacement therapy.
She was aware that sleep difficulties can be associated with the start of menopause. She was admitted for insomnia and a subsequent poor quality of life due to menopausal symptoms. She reported no trouble falling asleep but had difficulties maintaining that sleep. She reported going to bed at 8:00 PM and waking up at 8:00 AM.
However, she believed that she was sleeping only 6 hours per night, indicating either a misperception of the amount of sleep or long periods of staying in bed, which could be associated with depression. She also reported nocturia twice per night, with subsequent trouble in falling back to sleep. A general medical and a further gynecological examination found the patient to be within normal parameters. The medical evaluation revealed daytime tiredness, daytime sleepiness, a memory complaint, and a clinical diagnosis of sleep maintenance insomnia2 that had lasted for 4 months.
The study received prior approval by UNIFESP's ethical committee (approval No. 638.935/2014). Informed and written consent was obtained from the participant after explanation of the procedure had been given.
Procedures
At the first visit, an assessment of the patient's symptom history was taken, and a selection of the remedies corresponding specifically to her needs during the clinical interview with a specialist in Bach flower remedies was made. The selection was determined using the questionnaire scores, her complaints, personal characteristics, and emotional state. The blend followed the Bach emotional groups method, which consists of 12 healers (Agrimonia eupatoria and Gentianella amarella, the plants associated with the personality), 7 helpers (Olea europaea, associated with the person's chronic conditions), and second 19 (cherry plum, Larix decidua, Juglans regia, and Aesculus hippocastanum, plants to develop greater inner and focused on immediate issues).
After the initial session, the research team met with the participant and she was monitored during the next 7 sessions through clinical observation. She received further supplies of her same remedy at each session. The study was conducted for 4 months, with sessions taking place twice per month for 8 sessions. All the questionnaires were completed only at baseline and after intervention
To create the Bach flower remedy, 2 drops each of 7 ingredients in their concentrated forms were placed in a 30-mL bottle, diluted with 21 mL of mineral water and 9 mL of brandy, providing 30% alcohol by volume. The supplements were added in the following order: A eupatoria, G amarella, O europaea, cherry plum, L decidua, J regia, and A hippocastanum. They were prepared by the research team.
The patient completed the following subjective measures at baseline and postintervention for (1) anxiety, the Beck Anxiety Inventory (BAI)10; (2) depression, the Beck Depression Inventory (BDI)11; (3) quality of life at menopause, the Menopause Specific Quality of Life Questionnaire (MENQOL)12; (4) menopausal symptoms, the Blatt-Kupperman Menopausal Index (BKMI)13; (5) sleepiness, the Epworth Sleepiness Scale (ESS)14; (6) quality of sleep, the Pittsburgh Sleep Quality Index (PSQI)15; and (7) insomnia, the Insomnia Severity Index (ISI).16 The patient also underwent a polysomnography (PSG) exam prior to and after the intervention.
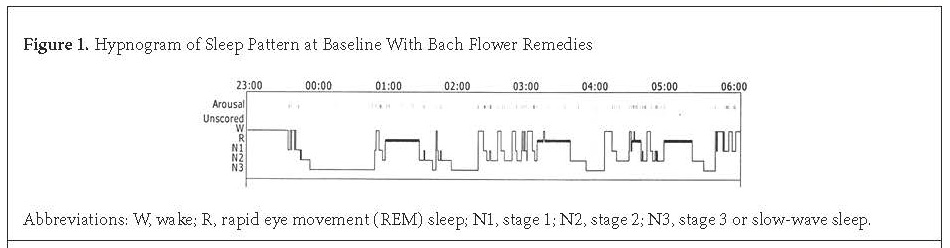
The PSG exams at baseline and postintervention were conducted at the Sleep Institute Clinic, respecting the usual time that the participant went to bed, and they were scheduled according to the patient's availability. She underwent a full night of PSG, which was performed using a digital system (EMBLAS7000; Embla Systems Inc, Broomfield, CO, USA). The 2 PSGs were visually scored by a registered and trained PSG technologist. All sleep stages were scored according to standardized criteria for investigating sleep.17 Electroencephalogram (EEG) arousals and leg movements were scored according to criteria established by the American Academy of Sleep Medicine (AASM) Manual for Scoring Sleep and Associated Events.18 Figure 1 shows a hypnogram, a graph that represents sleep architecture (the structure and pattern of sleep, including sleep duration, sleep depth, sleep stages, and sleep latency, as well as the organization of sleep cycle) of the participant at baseline.
Intervention
The prescription used the standard dose for the supplement (ie, 4 drops to be taken under the tongue, 4 times per day for 16 weeks). The blend that the participant received at each session was the same for all sessions and included multiple essences, such as (1) A eupatoria—used for individuals who keep their troubles hidden, presenting apparent happiness, and frequently used as a sleep aid; (2) cherry plum—used for individuals who show fear of their minds being overstrained and helps in providing mental and emotional control; (3) G amarella—alleviates mild downheartedness, acting as a remedy when things go wrong; (4) L decidua—used for individuals who show low self-esteem, feelings of inferiority, and/or a lack of confidence; (5) O europaea—used for individuals who lack vital energy and need to restore it and also helps to restore the faith and strength that one needs to continue an effort; (6) J regia—used for individuals who have difficulties in adapting to change and who suffer external influences from the present and the past; and (7) A hippocastanum—used for individuals who have unwanted thoughts and excessive worry that causes mental torment.
Outcome Measures
The PSG exams and the questionnaires (validated) were administered at baseline and postintervention (16 weeks).
Beck Anxiety Inventory. This 21-question multiple-choice and self-report inventory. BAI ask about common symptoms of anxiety (such as numbness and tingling, sweating not due to heat, and fear of the worst happening) that the subject has had during the past week (including the day the inventory is conducted). The scoring on the BAI is as follows: 0 to 7, minimum degree of anxiety; 8 to 15, mild anxiety; 16 to 25, moderate anxiety; and 26 to 63, severe anxiety.10
Beck Depression Inventory. This 21-question multiple-choice and self-report inventory. BDI ask about symptoms of depression, such as hopelessness and irritability; cognitions, such as guilt or feelings of being punished; and physical symptoms, such as fatigue, weight loss, and lack of interest in sex that the subject has had during the past week (including the day the inventory is conducted). The scoring on the BDI is as follows: 0 to 9, no depression symptoms; 10 to 15, mild depression symptoms; 16 to 19, mild to moderate depression symptoms; 20 to 30, moderate to severe depression symptoms; and >30, severe depression symptoms.11
Menopause Specific Quality of Life Questionnaire. This 29-itens in Likert-scale format has 4 domains of menopausal symptoms, as experienced in the last month (items: vasomotor, 1 to 3; psychosocial, 4 to 10; physical, 11 to 26; and sexual, 27 to 29). Improvement is when the range score decreases tending to 0.12
Blatt-Kupperman Menopausal Index. This 11-symptoms menopausal scale is rated on mild, moderate, and severe. The scoring on the BKMI is as follows: 0 to 17, mild; 18 to 34, moderate; ≥35, accentuated menopausal symptoms.13
Epworth Sleepiness Scale. This 8-item measure assesses the likelihood the individual will fall asleep during different situations. The scoring on the ESS is as follows: 0 to 9, no sleepiness symptoms, and >10, suggestive of daytime sleepiness and requires medical assistance.14
Pittsburgh Sleep Quality Index. This 19-item index (7 subscores are calculated including sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, sleep medication use, and daytime dysfunction) measures assessed sleep quality and disturbances during a 1-month interval. The scoring on the PSQI is as follows: 0 to 4, good sleep; 5 to 10, bad sleep; and >10 requires medical assistance.15
Insomnia Severity Index. In this 7-question self-report, the answers are added up to calculate a total score. The scoring on the ISI is as follows: 0 to 7, no clinically significant insomnia; 8 to 14, subthreshold insomnia; 15 to 21, clinical insomnia—moderate severity, and 22 to 28, severe clinical insomnia.16
Polysomnography. This is multiparametric test used in the sleep study and monitors many physiological body functions, including brain (EEG), musculoskeletal activation (electromyography), eye movements (electrooculogram), and heart rhythm (electrocardiogram) during sleep. PSG show all the sleep stages through a graphic, the hypnogram, which represents sleep architecture (the structure and pattern of sleep, including sleep duration, sleep depth, sleep stages, and sleep latency, as well as the organization of sleep cycle). Each sleep cycle last from approximately 90 to 120 minutes, and a given night has 4 to 6 different sleep cycles; it shifts between the different sleep stages (such as nonrapid eye movement [NREM] and rapid eye movement [REM] sleep) as well as arousal to wakefulness. NREM sleep consists of N1 sleep (the lighter sleep stage); N2 and N3 sleep (slow-wave sleep, deeper than N1); and REM sleep, which is the deepest state of sleep. These stages shift during the night.17,18
RESULTS
The patient's insomnia improved, with the ISI showing a change from severe clinical to subthreshold insomnia (Table 1), despite an objective PSG finding that indicated an increase in sleep fragmentation (ie, waking after sleep onset) and a decrease in sleep latency (Table 2). However, the PSG also indicated an increase in sleep efficiency.
The PSG exam is not the preferable exam to measure insomnia, because it measures only 1 night and, in the current case, an actigraphy performed for a minimum of 10 days would have been preferred. The patient presented no sleepiness symptoms before and after treatment (Table 1). The research team speculates that the subjective sleep parameters could have been improved secondarily by a reduction in anxiety and nervousness after the treatment with the Bach flower remedies.
Regarding menopausal symptoms, the supplement improved all constructs on the MENQOL (ie, vasomotor, psychosocial, physical, and sexual) (Table 1). Anxiety symptoms on the BAI also showed improvement after treatment, with the patient's anxiety decreasing from moderate to mild (Table 1).
Table 1. Comparison of Participant's Subjective Measurements of Sleep, Menopausal Symptoms, Anxiety, Depression, and Quality of Life Before and After Bach Flower Therapy
The scoring on the questionnaires is as follows:
ISI: 0–7, no clinically significant insomnia; 8–14, subthreshold insomnia; 15–21, clinical insomnia—moderate severity; 22–28, severe clinical insomnia.
ESS: 0–9, no sleepiness symptoms; ≥10, suggestive of daytime sleepiness and requires medical assistance.
PSQI: 0–4, good sleep quality; 5–10, poor sleep quality; >10 requires medical assistance.
BKMI: 0–17, mild; 18–34, moderate; >35, accentuated menopausal symptoms.
BAI: 0–7, minimum degree of anxiety; 8–15, mild anxiety; 16–25, moderate anxiety; 26–63, severe anxiety.
BDI: 0–9, no depression symptoms; 10–15, mild depression symptoms; 16–19, mild to moderate depression symptoms; 20–30, moderate to severe depression symptoms; >30, severe depression symptoms.
MENQL: Improvement has occurred when the score decreases, tending to 0.
|
Preintervention |
Postintervention |
ISI |
22 |
10 |
ESS |
3 |
2 |
PSQI |
14 |
9 |
BKMI |
16 |
10 |
BAI |
19 |
11 |
BDI |
6 |
3 |
MENQOL |
|
|
Vasomotor |
4 |
1 |
Psychosocial |
4.57 |
2.71 |
Physical |
6.19 |
3.38 |
Sexual |
2.66 |
1.33 |
Abbreviations: ISI, Insomnia Severity Index; ESS, Epworth Sleepiness Scale; PSQI, Pittsburgh Sleep Quality Index; BKMI, Blatt-Kupperman Menopausal Index; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; MENQOL, Menopause Specific Quality of Life Questionnaire.
Table 2. Comparison of Objective Measurements From Polysomnography of Sleep Pattern Before and After Bach Flower Therapy
|
Preintervention |
Postintervention |
Sleep latency (min) |
36.7 |
7.2 |
REM sleep latency (min) |
83.5 |
79 |
Total sleep time (min) |
341.0 |
355.5 |
Sleep efficiency (%) |
79.5 |
85.6 |
Stage N1 (%) |
12.6 |
13.6 |
Stage N2 (%) |
28.5 |
52.3 |
Stage N3 (%) |
31.7 |
9.8 |
REM sleep (%) |
26.2 |
25.2 |
Arousal index (number/h) |
13.9 |
9.8 |
WASO (min) |
51.5 |
52.6 |
PLM index (number/h) |
0 |
1.4 |
AHI (number/h) |
5.8 |
4.2 |
Baseline SaO2 (%) |
96.3 |
95 |
Mean SaO2 (%) |
94.7 |
94.3 |
Minimum SaO2 (%) |
85.0 |
86.0 |
Abbreviations: REM, rapid eye movement; WASO, wake after sleep onset; PLM, periodic leg movements; AHI, apnea-hypopnea index; SaO2, oxygen saturation level.
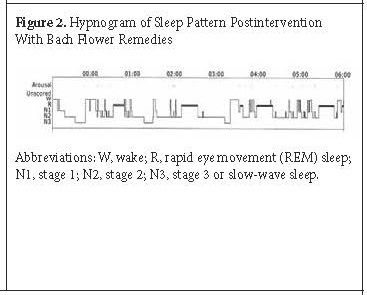
Regarding the objective findings of sleep from the PSG, the research team noted a change in the participant's sleep architecture (Table 2). Figure 2 shows a hypnogram of the participant's sleep pattern postintervention.
Like sleep latency itself, the participant's REM sleep latency decreased postintervention. Both variables moved into normal sleep parameters. Among the sleep stages, stage N2 NREM clinically improved because it increased. Stage N3 NREM diminished, probably due to a new arrangement in the sleep architecture. Finally, stage N1 NREM and stage REM sleep were almost the same.
The arousal index and the apnea-hypopnea index on the PSG both decreased, indicating improvement in both parameters. The participant's sleep duration was longer as can be seen in the increase in the total sleep time compared to the length before treatment.
Collectively, the findings indicated an overall positive change in the participant's sleep architecture due to the treatment with Bach flower remedies. In this case, changes in the objective measures of sleep were clinically significant due to the decrease in sleep latency as well as the increase in sleep efficiency and its subjective improvements. Moreover, diurnal repercussions from insomnia, such as daytime sleepiness, daytime tiredness, memory, and insomnia complaints also improved.
DISCUSSION
In the current case report, the research team evaluated the effects of Bach flower remedies on sleep patterns and menopausal symptoms of a postmenopausal patient diagnosed with insomnia. To the team's knowledge, its report is the first investigating the supplement's effects on objective sleep parameters. No specific investigations have occurred in the past on the supplement's effects on sleep disorders, especially insomnia, using a multimodal sleep assessment (ie, both the PSG and the sleep questionnaires).
The use of the supplement in menopausal symptoms has been evaluated previously by 2 studies.6,8 Like the current study, Docalet al6 demonstrated improvements in menopausal symptoms, such as irritability and anxiety, when the supplement was used for 25 days. As did the current study, Lopez-Suarez et al8 investigated insomnia and psychological symptoms, such as anxiety and depression, in menopausal transition and postmenopause. They found that the frequency of anxiety, depression, and insomnia in participants was 48.3%, 43.3%, and 46.7%, respectively. After 6 months of the intervention, those symptoms improved by 96.1%, 93.1%, and 82.1%, respectively.8
The supplement improved the participant's menopausal symptoms (ie, vasomotor, psychosocial, physical, and sexual) (Table 1). Others studies have demonstrated improvements in vasomotor and psychological symptoms in postmenopausal women8 and specifically in anxiety and stress,6 with no secondary reactions.7 Postmenopausal women experience depressive symptoms, anxiety, irritability, nervousness, low self-esteem.9,19 In the current study, anxiety symptoms improved after treatment, decreasing from moderate to mild anxiety (Table 1).
The current study is an additional step in the direction toward treatment of postmenopausal women with complementary medicine. Additional studies are warranted to investigate primary and secondary effects as well as the mechanisms of the Bach flower remedies on sleep parameters and menopausal symptoms.
CONCLUSIONS
In the current case study, the use of Bach flower remedies improved the patient's emotional state, addressed negative physiologic changes, and changed the patient's sleep architecture. Although it is difficult to draw a definitive conclusion as to the therapeutic value of the essences, the results were encouraging. The indication of Bach flower remedies as a therapeutic strategy to relieve menopausal symptoms, such as anxiety, mood changes, and insomnia, seems worthy of further investigation in a larger sample size.
ACKNOWLEDEGMENTS
The study was supported by grants from Associação Fundo de Incentivo a Pesquisa. Three of the research team are recipients of fellowships from the National Council for Scientific and Technological Development in Brazil. Another team member is a recipient of funding from the São Paulo Research Foundation (No. 2014/18722-5).
AUTHOR DISCLOSURE STATEMENT
The authors declare that they have no conflicts of interest.
REFERENCES
Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife. Menopause. 2003;10:19-28.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Hachul H, Garcia TK, P Maciel AL, Yagihara F, Tufiki S, Bittencourt L. Acupuncture improves sleep in postmenopause in a randomized, double-blind placebo-controlled study. Climacteric. 2013;16:36-40.
Llanas AC, Hachul H, Bittencourt LRA, Tufik S. Physical therapy reduces insomnia symptoms in postmenopausal women. Maturitas. 2008;61:281-284.
Oliveira DS, de Campos HH, Goto V, Tufik S, Bittencourt LRA. Effect of therapeutic massage on insomnia and climateric symptoms in postmenopausal women. Climateric. 2012;15:21-29.
Docal BP, Mengana MJ, Garcia EM, Contreras A JD. Terapia floral y climateriofemenino. Rev Cubana Plant Med. 2006;11:3-4.
Mesa YL, Garcia TIN. Terapia floral en síntomasclimatéricos. Rev Cubana Obste Ginecol. 2002;28:111-119.
Lopes-Suaréz JC, del Toro MosqueraGlA, Cordero LP, Zamora YC, Posada YF. La Terapia Floral de Bach en el tratamiento del sídromeclimaterico feminine/ Bach flower therapy in the treatment of female climacteric syndrome. Med Ciego 2011;1 (Suppl 1):
LaTorre MA. Intergrative perspectives. Integrating Bach flower remedies into a therapeutic practice. Perspct Psychiatr Care. 2006;42:140-143.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psych. 1988;56:893-897.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561-571.
Hilditch J R, Lewis J, Peter A, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996;24:161-175.
Kupperman HS, Wetchler BB, Blatt MHG. Contemporary therapy of the menopausal syndrome. J Amer Med Assoc. 1959;171:1627-1629.
Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540-545.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297-307.
Rechtschaffen A, Kales A. A manual of standardized terminology: Techniques and scoring system for sleep stages of human subjects. Los Angeles, CA: Brain Information Service/Brain Research Institute; 1968.
Iber C, Ancoli-Israel, Chesson A, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules terminology and technical specifications. Westchester, IN: American Academy of Sleep Medicine; 2007.
Masi Mark P. Bach flower therapy in treatment of chronic major depressive disorder. Alternative Ther Health Med. 2003;9(6):108-110.
